Chronic pain is the most common reason people seek medical help. Up until recent years, physical pain was thought to be isolated in the body with no correlation to emotional pain. Scientists are now finding that there is a strong connection between the two. The same part of the brain, the neural system, processes both types of pain; meaning the sensations we experience for both physical and emotional pain travel the same neurological pathways.
Studies have shown that people who have experienced both physical and emotional trauma can experience more severe symptoms of each type of distress than those who have experienced only one kind of trauma.
Understanding the connection is important to medical and mental health professionals as they work with patients to explore the causes of their pain and treat it effectively.
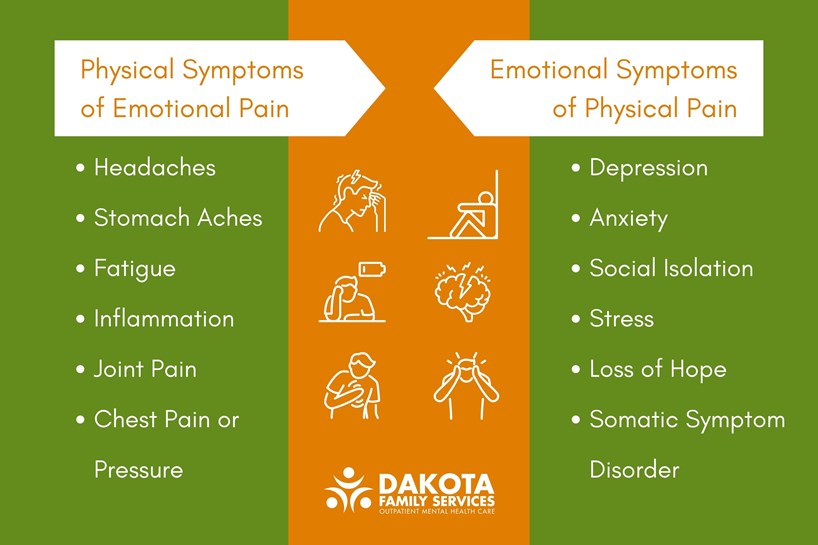
The Physical Symptoms of Emotional Pain
Emotional trauma can lead to physical symptoms like headaches, stomach aches, fatigue, and joint pain.
For instance, it's common for people suffering from depression to also experience joint pain. When you are depressed, the neurotransmitters change, causing a cascade of symptoms that include inflammation, which manifests as joint pain.
Anxiety is commonly linked to headaches and digestive issues. And, when anxiety leads to a panic attack, physical symptoms include dry mouth, increased heart rate, shortness of breath, and numbness in hands and feet.
It's no coincidence that the phrases "soul-crushing" or "heart-wrenching" often accompany discussions of emotional pain. When you've experienced a painful breakup, for example, your heart can feel like it's being crushed. And if you've ever been injured in a car accident, then lost your job on top of that, you might know what "soul-crushing" means. It's not just a metaphor—emotional pain is real and can be as painful as physical pain.
While you can experience pain anywhere in your body, the most common location for emotional distress to manifest as physical symptoms is in the stomach. This is because our brains can't differentiate between real and imagined pain. So, if you're worried about something that hasn't happened yet or if you're stressed about something that already happened, your brain essentially sends a signal to your stomach that it's in trouble. That's why people often get an upset stomach when they're nervous or anxious—their brain thinks there's danger coming and sends signals to their organs to prepare.
The Emotional Symptoms of Physical Pain
When you're suffering from physical pain, it can be easy to ignore your emotional state. But the two are connected—and ignoring them both can make things worse.
If you are suffering from chronic pain, you may worry about the future, lose hope, and feel like a burden to others. This can lead to depression, anxiety, and social isolation, which in turn may increase your sensitivity to pain. If you have an accident or a stroke, you may be worried about how your injury or illness will affect your quality of life, income, relationships, or family. These thoughts and emotions cause stress, and the body's response to stress is to release cortisol, which can make you feel even more anxious and depressed.
In some cases, physical pain can lead to Somatic Symptom Disorder, a mental health condition characterized by an abnormal focus on physical symptoms that leads to major distress or problems functioning. Some people with this disorder have been diagnosed with medical conditions, but the thoughts, feelings, and behaviors related to the illness are out of proportion. For others, medical conditions have been ruled out and there is no clear diagnosis for the symptoms. Because physical conditions may not be the root cause of the pain, this disorder is sometimes difficult to diagnose and can be very challenging for patients and their medical and mental health clinicians.
A Dual Approach to Treatment
Because of the overlap of physical and emotional pain, patients often benefit from working simultaneously with both medical and mental health providers. You can start with your physician or a mental health provider, whatever is most comfortable for you.
If you see a mental health professional, they will likely ask questions about your medical and physical health conditions and symptoms. At Dakota Family Services, we believe it’s important to get the whole picture and when appropriate, refer you back to your doctor to rule out significant medical conditions. If I’m treating you for depression and you have mononucleosis or a thyroid condition, you won’t be able to make any progress until the underlying medical issues are treated as well.
Sufferers of chronic pain most often begin with their medical provider. Your treatment will depend on the underlying reason for the pain and may include medication, physical therapy, surgery, and implantable electrical stimulators.
Because most doctors who treat chronic pain recognize the connection between emotional and physical pain they will also recommend psychological therapy to help you learn how to cope with your condition. This can include learning about stress management and relaxation techniques as well as identifying triggers for your pain that may be emotional or physical in nature (or both).
Some psychological treatment modalities used to treat patients suffering from chronic pain include Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), Acceptance and Commitment Therapy (ACT), and Mindfulness-Based Stress Reduction Therapy (MBSR).
- CBT will help you look at the way your thoughts develop from your experiences. How you think about yourself and how you respond to the words and actions of the people around you are often automatic and based on prior experiences. CBT can help you shift your perspective and perception so you can choose other ways to respond to situations that cause you distress.
- DBT is another form of therapy that helps you change thoughts and behaviors that get in the way of reaching your goals or living your best life. Using the DBT tool of distress tolerance, you can learn to accept and tolerate your pain. It might seem counterintuitive, but a strategy of balancing acceptance and change can help you shift your energy from avoiding and ignoring your pain to discovering and focusing on the positive aspects of your life. Other pillars of this modality include mindfulness, interpersonal effectiveness, and emotion regulation, which all help patients cope with pain.
- ACT is another type of therapy that includes mindfulness. It can help a person accept thoughts and experiences as they are rather than trying to change them.
- MBSR is a meditation and yoga-based therapy. Originally designed for stress management, it is also used to treat a variety of illnesses such as depression, anxiety, chronic pain, cancer, diabetes mellitus, hypertension, and skin and immune disorders. During MBSR, patients learn stress reduction and relaxation techniques to manage symptoms.
Other therapies also considered include Biofeedback, Eye Movement Desensitization and Reprocessing (EMDR), Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), Hypnosis, Somatic Anchoring, and Hyperbaric Oxygen Chamber Therapy.
Don't Suffer in Silence
If you are struggling with emotional or physical pain, don't be afraid to get help. It's not only important to get treatment for your condition—but also to find ways to cope that will help mitigate the effects on your body and mind. Combining therapy with other chronic pain treatment options is the best way to alleviate your pain.
Don't give up until you get answers or relief!


